Cancer results from a combination of spontaneous mutations that arise with age—just call it “bad luck”—and environmental exposures to carcinogens such as tobacco, ultraviolet light or viruses. But the question of the relative contribution of luck—compared with more explicit causes—has generated vigorous debate for years.
The distinction matters because of the implications for cancer prevention: If a cancer is mostly caused by toxic exposures, then public health efforts should focus on strategies to prevent those exposures. But if a cancer is mostly the result of random mutations, then little can be done to prevent it, and efforts might instead focus on early detection and treatment.
Now a team of researchers has addressed this ongoing controversy with a degree of mathematical exactitude. Biostatistician and evolutionary biologist Jeffrey Townsend of Yale School of Public Health, Vincent Cannataro of Emmanuel College and Jeffrey Mandell of Yale devised a method inspired by evolutionary models of natural selection in wild populations to quantify how much every so-called point mutation, or change to a single DNA letter, in a tumor contributes to driving its growth.
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing. By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
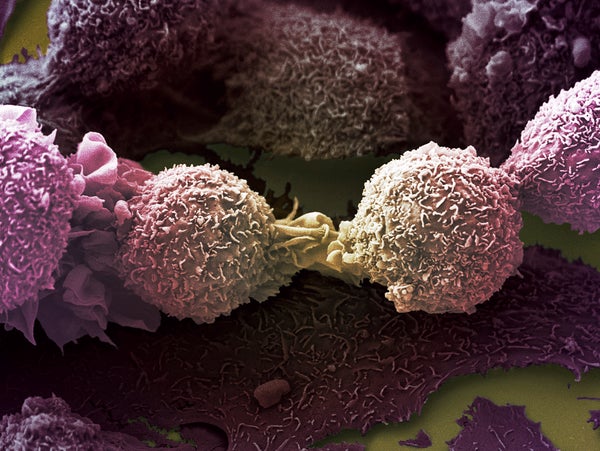
Inside a tumor, there are usually many genetic mutations, but only a small subset of them “drive” cancerous growth. The rest are harmless “passenger” mutations. Using previous knowledge about the specific mutational patterns caused by exposures to carcinogens such as tobacco smoke or UV light, the researchers could estimate what proportion of driving mutations were caused by carcinogens and what proportion arose from accidental alterations in DNA that occur during normal cell division.
In the study, appearing in Molecular Biology and Evolution on April 26, the researchers used this method to investigate the causes of point mutations in 24 major cancer types. For each type, they were able to estimate how many cancer-driving mutations were linked to “bad luck.” Confirming epidemiological studies, they found that melanomas and lung, bladder and cervical cancers are largely attributable to exposure to carcinogens such as UV light, tobacco or human papillomavirus, whereas brain and spinal cord tumors called gliomas and prostate tumors called adenocarcinomas are mostly the result of intrinsic mutations that accumulate with age.
The study “is a step forward because it’s allowing a better assessment of the particular contribution of the agent— smoking, UV, et cetera—toward the actual driving mutations,” says James DeGregori, a cancer researcher at the University of Colorado School of Medicine, who was not involved with the study. “Let’s say you have a lung cancer with five driver mutations—you can say, ‘These three clearly have the smoking signature, so they were directly caused by the smoking.’”
“There have been a lot of sidetracks taken over the years,” says cancer researcher and oncologist Rameen Beroukhim of the Dana-Farber Cancer Institute, who was not involved with the new study, because people assumed that frequently mutated genes in a given cancer type must be contributing to the development of the cancer—only to find out that those mutations were just passengers. It has been important to understand the signatures of different mutational processes, but therapeutically, what Beroukhim and his colleagues are interested in is the small subset of mutations that are causing the cancer to grow.
For this reason, it has been tricky to pin down the definitive causes of a given cancer. And until now, the discussion has focused on risk factors—estimated over population averages—that could have contributed to the development of a tumor. Townsend says his team’s new approach can be used to pin down the proximate causes of the driving mutations in a given patient’s tumor and thus provides a more precise answer to one of the most difficult questions that patients and doctors struggle with after a cancer diagnosis: “Why me?”
One caveat of the study is that the researchers focused only on mutations in single letters, or nucleotides, of DNA, not large rearrangements of chromosomes or increases in copies of a gene that frequently occur in cells as they become cancerous. The reason is that the researchers did not have a way to quantify the selective effect of those large mutations in their evolutionary models, although they are working on methods to address that problem now.
These large mutations are not negligible in cancer cell genomes: in some cancers, one out of every 10 million nucleotides undergoes a point mutation, but one of every three is involved in chromosomal rearrangements or increases in copy numbers, Beroukhim says. Still, it is unclear how much these big rearrangements contribute to cancer growth because they have yet to be quantified for individual cancers.
Townsend acknowledges that the findings are limited because they do not take into account these large changes in the genome. It is possible, he says, that the percentage of point mutations caused by environmental exposures, as opposed to intrinsic factors, is approximately the same for these other types of mutations, so the conclusions would largely be the same. But that hypothesis still must be confirmed. “We’ll learn in the future, but this is our first way of doing it,” Townsend says.
In addition, determining causality in cancer remains a complex task. If a cancer-driving mutation does not have the signature of a carcinogen exposure, that does not mean that the carcinogen did not contribute to the cancer; it means it did not contribute to that mutation, DeGregori points out. The environmental exposure may have been indirectly responsible for promoting the development of the cancer by changing the mutated cell’s environment, he argues. For example, smoking changes the environment in a smoker’s lung, so a mutated cell inside that lung would behave differently than the same cell in a healthy nonsmoker’s lung. The environment of a cell will influence its behavior and its ability to proliferate.
Townsend agrees that this context is important: in the same way, obesity, exercise or alcohol consumption may not directly cause (or prevent) mutations, but these factors change the metabolic environment in the body and thereby alter the risk of cancer, too. Future work will need to incorporate this larger context. Future work will also extend to more cancer types as more cancer genomes are sequenced and become available.
Despite these limitations, this novel method could provide insights into the age-old problem of cancer resistance to treatment: Frequently, a tumor will initially respond to treatment but come back after some time. That is because many chemotherapies themselves are mutagenic. The hope is that the mutations will be more damaging to cancer cells, which often lack good DNA repair mechanisms, than to healthy cells. But some of those treatment-caused mutations may enable the tumor to evolve resistance to treatment. Townsend and his colleagues recently used their evolutionary model to pin down exactly which mutations caused by treatment in a given tumor are responsible for the resistance to that treatment—thus informing which combinations or sequences of treatments to use or avoid.
The method’s ability to address what causes cancer at the level of individual patients—something that had not been possible before—means that it could be extremely useful in legal cases, the researchers say. For example, it is typically very difficult to prove that a cluster of cancer cases in a community was caused by exposure to pollution or a toxic waste site nearby. But using this method to look at the tumors of cancer patients could establish causal links between exposure and a specific patient’s tumor, which could have implications for legal liability.
“If this would have been available back when the tobacco lawsuits were going on, this would have been an incredibly useful, to be able to say, ‘Here’s the signature of tobacco smoking on all of these patients’ tumors; you can’t say that this is just some side effect,’” Townsend says. “It’s nice to have a direct link between the tumor itself and the mutagens that caused it.”