A doctor would be foolish to conclude that a patient’s heart and lungs are healthy merely because they show up alive to the medical office. That’s why doctors routinely use a stethoscope to listen for abnormalities, and why they measure heart rate, blood pressure and oxygenation in blood, assess blood cell compositions and blood chemistry, and apply EKG and other simple functional indices of cardiovascular-pulmonary health at regular checkups, to head off future problems.
In contrast, there is little serious attempt in everyday medicine to manage organic brain health. Even though a majority of people are challenged by a life-degrading neurological or psychiatric illness across a significant span of their lives, there’s no equivalent of a stethoscope, blood pressure cuff or EKG to routinely assess brain health during a visit to the doctor. Doctors usually assume that a patient’s brain is healthy when they walk into the clinic, hold a conversation, and appear to be sustaining themselves on an elementary, functional level.
We’re beginning to move into a new era in medical practice, one focused less on treating diagnosed illness and more on broad informative assessments and health management strategies supporting wellness. We now have tools that enable the routine assessment of brain health in a clinical setting. And we are rapidly working toward the day when we can draw on vast amounts of historical and current personal data to reliably record early warning signs that point to future neurological and psychiatric illness. There is every indication that, by paying closer attention to brain health and intervening at the first signs of trouble, we will be able to prevent a substantial majority of neurological and psychiatric illnesses.
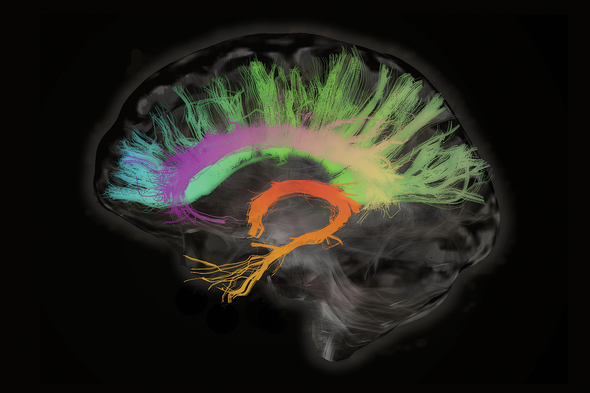
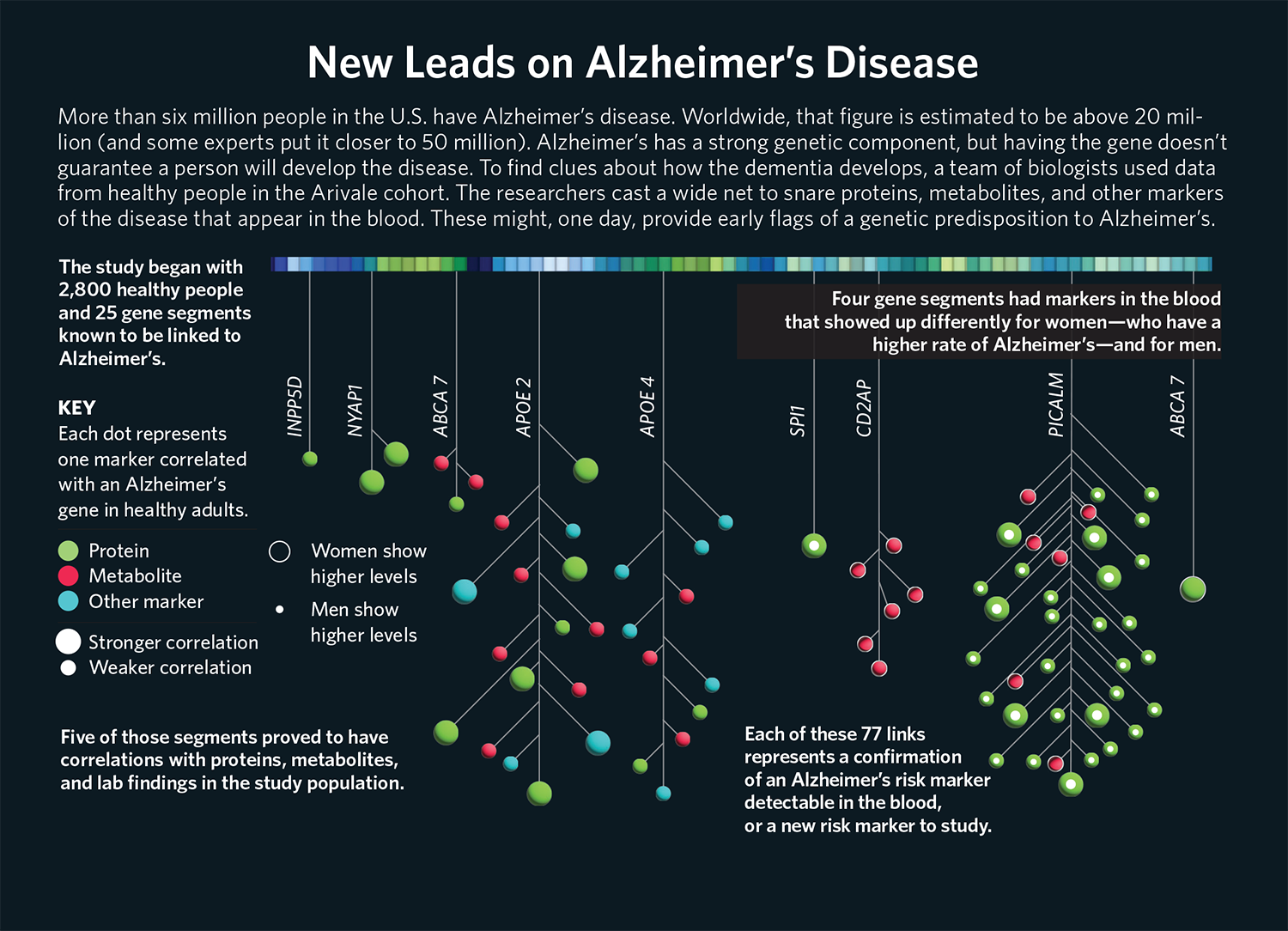
Our ability to analyze and update a broad range of brain-health-relevant information is rapidly progressing. That information includes data on a person’s genomics, gene expression, body chemistry. It includes that person’s medical history, which can be largely provided by the doctor’s office. It includes documented life history factors that impact brain health, as well as data on neurological performance that is collected using computerized assessments and wearable sensors. When integrated and subjected to appropriate AI analytics, these data will be highly informative about the status of our neurological well-being.
To explore these new opportunities, our team at Posit Science—a company that I co-founded in 2014 to translate research advances around brain plasticity into new tools to support brain health assessment and neurological resilience, recovery and optimization—has been working with scientists at Phenome Health. Together we’re working to address the remaining challenges to full implementation of this next-gen medical model.
Assessing Brain Health
Two challenges stand in the way of routine clinical assessments of brain health. First, while medical scientists have developed many highly sophisticated technologies for assessing the physical and functional status of the brain, practical, scalable tools have not yet made it out of the laboratory into routine clinical practice. Second, the blood-brain barrier—a tight junction barrier in capillaries that keeps blood-based infectious agents and larger chemical molecules out of brain tissues—limits the detection in blood samples of chemical indicators from the brain that could foretell future neurological decline or dysfunction.
Counterbalancing these two disadvantages, there are two major advantages for the brain compared to other organs that support the effective management of its health. First, we have low-cost ways, using scalable computerized assessment strategies, to identify neurological weakness or distortion, and can now relatively rapidly construct a risk index for a progression to psychiatric or neurological illnesses. For example, we can easily document the speed and accuracy of neurological operations in a patient’s brain. Those indices inform us about the physical state of information processes in the brain because, in general, fast and accurate brains are necessarilyphysically advanced—strongly connected, with well-insulated transmission lines, with highly reliable and stable information transmission, recognition, memory, reasoning and executive control processes. We can also rapidly index the neurological processes governing attention control and the social and emotional brain in ways that inform us about neurological limitations or distortions that, in the untreated patient, foretell possible downstream psychiatric and neurological disasters. These same assessments also index the status of the machinery of the brain that controls brain plasticity itself, which equates with the patient’s capacity for exercise-driven strengthening and recovery.
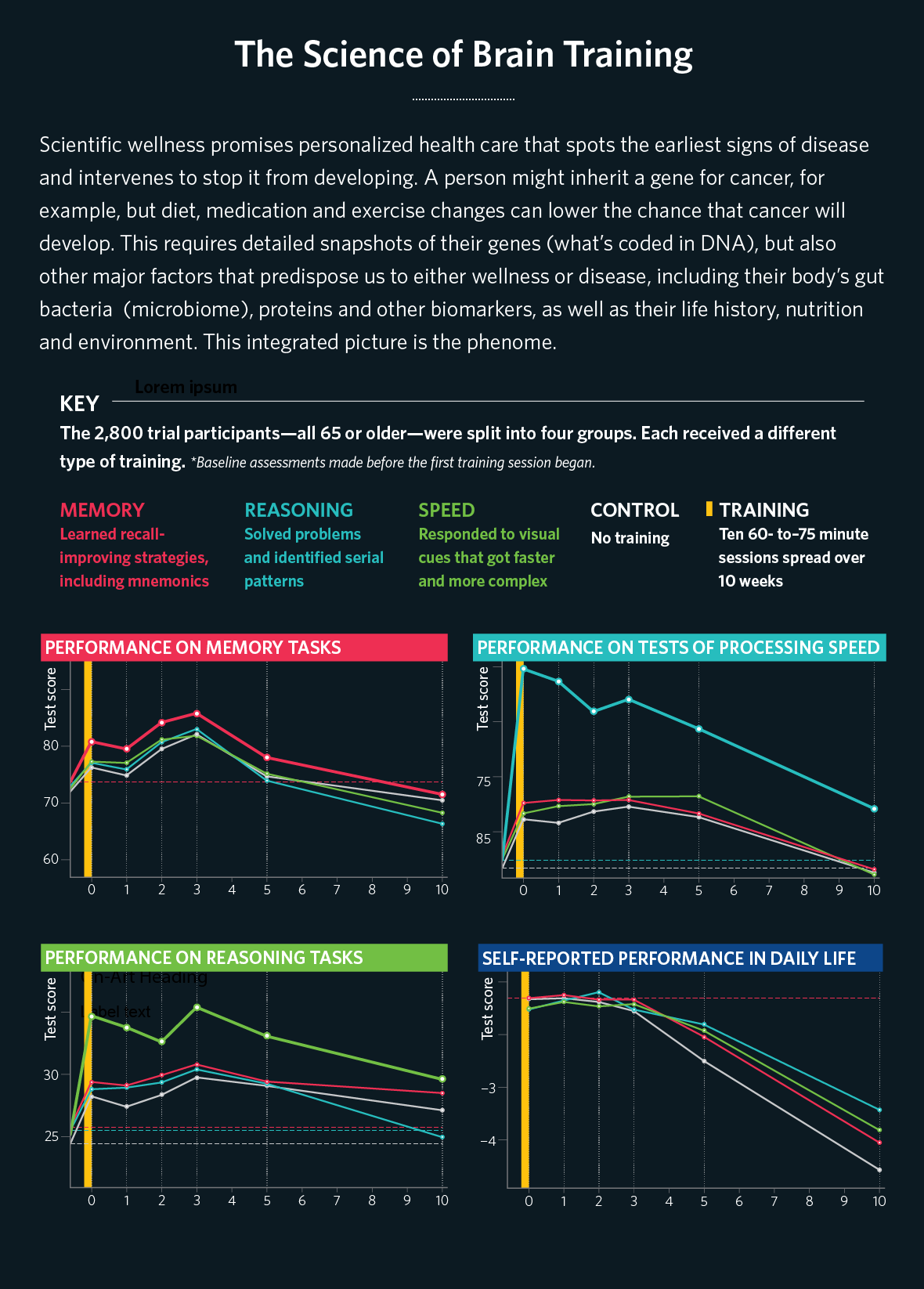
Second, we know from a growing number of studies that an advanced state of brain health is a consequence of specific forms of brain engagement, or brain exercise. The brain is like the physical body. When you exercise it in appropriate ways, everything that supports its growing functionality—including, for example, its blood supply, its intracellular metabolic support, its connectional strength and reliability, the machinery that supports its plasticity, and the powers of its immune response, among a long list of other documented positive impacts—all strengthen in parallel. Like an appropriately exercised physical body, a fast and accurate and reliably controlled brain is necessarily broadly healthier, and, in general, a sluggish and inaccurate brain and impulsive brain is not physically healthy.
Because a simple index of brain speed and accuracy, for example, strongly implies the parallel status of that long list of physical, vascular, metabolic, immune system and other indices of organic brain health, it can provide clinicians and patients with a powerful simple index of organic brain health. A patient, in a routine clinical visit, can easily complete an assessment of brain speed and accuracy in vision, hearing and action control integrated with broader indices of attention, memory, executive control, and social and emotional balance and control.
These tools have a diagnostic value for evaluating brain health that are at least equivalent to the multiple measures now used to routinely assess the status of cardiopulmonary health. There is simply no excuse, in modern clinical practice, to continue to assume that someone’s brain is healthy just because its owner is capable of basic behavioral functioning, any more than it is reasonable to assume that a patient’s heart is healthy just because it is beating.
This new class of brain assessments supports Phenome Health’s broader wellness approach. The data they generate will be integrated with data from genomics, gene expression, blood chemistry, clinical records, personal history records, and wearable sensor data. Through AI analysis, these data will inform medical practitioners about brain health and its intelligent management. Any indication of emergent weakness or distortion in brain function is a wellness target, and in most of these domains, our highly plastic brain has the capacity to grow its powers using these powerful next-gen tools.
The Promise of Managing Brain Health
Our neurological health status and the abilities that define our operational personhoods arise from our “plastic” brains, molded by our experiences. Every skill and ability that defines that operational personhood is subject to strengthening or refinement at any age, as personal circumstances evolve. Conversely, gradual diminishment of brain plasticity underlies many neurological and psychiatric disorders. The good news is that we understand how to monitor the brain’s health in ways that inform us about how to intervene at the first signs of weakness or decline to put us on a path to sustained wellness.
To cite one of many examples of a functional index related to health, “cognitive reserve” processing speed with sustained accuracy—offers a measure of resilience against progression to Alzheimer’s disease and other dementias. That is another way of saying that faster and more accurate brains—which we have noted earlier are healthier brains—are less likely to progress to disease. Who’s surprised?
It’s relatively easy to engage almost any brain in training that accelerates its operational speed and advances its accuracy and reliability. For example, Posit Science has built a suite of progressive training programs accessed in a computerized “brain gym” designed to rejuvenate brain health. Using this system, called BrainHQ, the average 70-year-old’s brain can be trained to match or exceed the performance abilities of an average 30-year-old. Even a very limited dose of such training for individuals in the last decades of life results in broad improvements in neurological fitness, and in a substantially delayed or reduced probability of progression to dementia or other neurological illnesses.
We are now poised to enter a new era of brain medicine in which we track organic brain health and neurological performance, combine it with phenomic analysis, and respond to signs of emergent weakness or distortion with the full arsenal of wellness and treatment approaches. Lifestyle adjustments and brain fitness training will be the first line of defense for restoring and sustaining the brain’s organic health. These interventions will be backed up, when necessary, by pharmaceutical treatments, medical devices, and surgery. The outcomes of all of these approaches will be documented and analyzed using artificial intelligence.
Most neurological and psychiatric illnesses arise in brains at risk for progressive collapse. Most illnesses are end-stage conditions that develop after an extended period marked by multiple early-warning signs. As the medical world begins to actively manage brain health, we will discover, in this scientist’s opinion, that most of the psychiatric and neurological “diseases” that have plagued humankind across the ages are preventable. There is absolutely no question that almost everyone can be safer and happier when we bring this science to bear to help strengthen and sustain this most prized of human possessions—our powerful brains.
Michael Merzenich is co-founder and Chief Scientific Officer of Posit Science, a professor emeritus neuroscientist at the University of California, San Francisco, and author of Soft-Wired: How the New Science of Brain Plasticity Can Change Your Life.
Find out more about Phenome Health’s efforts to transform the future of health care here. Learn more about phenomics, the new science of wellness, in other stories in this special report.