If pimples are caused by oily skin, why doesn't a good washing prevent all breakouts? A recent study offers an answer— and maybe a new line of defense.
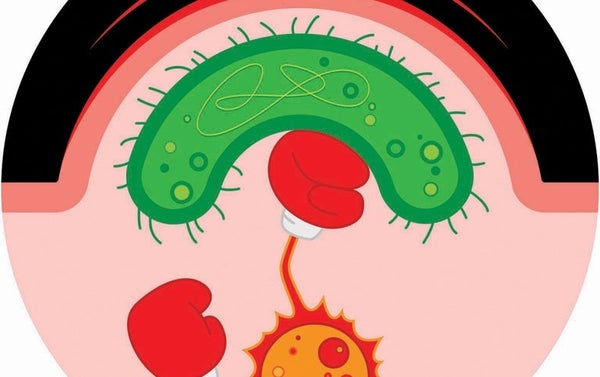
Pimples contain tiny and discrete bacterial infections. The most commonly involved bacteria are Cutibacterium acnes, which live innocuously on skin cells but can grow out of control when the skin's oily sebum increases and boosts bacterial food supply. What we think of as acne—the pustules, redness and swelling—is a battle between our immune system and these rapidly multiplying bacteria, says dermatologist Richard Gallo of the University of California, San Diego, who led the new study. “For most people, it's not that you're dirty, or you're not washing your face enough,” Gallo explains. “This is a problem with the way your body's immune system is dealing with the bacteria that are supposed to be there.”
If one imagines the immune system and bacteria as being on opposing soccer teams, acne is the beat-up turf at the end of the game. The new study identifies a previously unknown, and particularly turf-mangling, immune system player. Gallo and his colleagues showed in Science Translational Medicine that a structural cell type called a fibroblast (which is not typically considered an immune cell) contributes to the facial face-off. Working with mice and with human skin samples, the scientists found that C. acnes triggers fibroblasts to transform into fat cells that secrete an antimicrobial substance—along with inflammation-causing proteins. The researchers also discovered that retinoids, a powerful and commonly used class of pimple-fighting drug, work partially by blocking fibroblasts' transformation and release of irritating proteins.
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing. By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
Jonette Keri, a clinical dermatologist at the University of Miami Miller School of Medicine, who was not involved in the research, calls the finding an “exciting” new way to think about acne. Because retinoids can have undesirable side effects, she says, pursuing a more targeted way to stop the fibroblasts' transformation would be “fantastic” for clinical treatment.